
Learn how to diagnose and treat hyperlipidemia with these printable medical flash cards.
There are 18 flash cards in this set (3 pages to print.)
To use:
1. Print out the cards.
2. Cut along the dashed lines.
3. Fold along the solid lines.
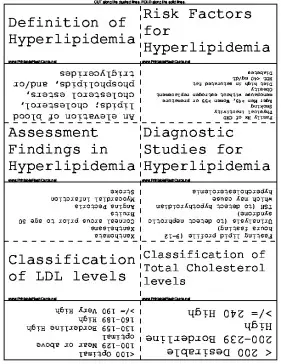
Sample flash cards in this set:




| Questions | Answers |
|---|---|
| Definition of Hyperlipidemia | An elevation of blood lipids; cholesterol, cholesterol esters, phospholipids, and/or triglycerides |
| Risk Factors for Hyperlipidemia | Family Hx of CHD Physical inactivity Smoking Age: Men >45, Women >55 or premature menopause without estrogen replacement Obesity Diet high in saturated fat HDL <40 mg/dL Diabetes |
| Assessment Findings in Hyperlipidemia | Xanthomata Xanthelasma Corneal arcus prior to age 50 Bruits Angina Pectoris Myocardial infarction Stroke |
| Diagnostic Studies for Hyperlipidemia | Fasting lipid profile (9-12 hours fasting) Urinalysis (to detect nephrotic syndrome) TSH (to detect hypothyroidism which may cause hypercholesterolemia |
| Classification of LDL levels | <100 Optimal 100-129 Near or above optimal 130-159 Borderline High 160-189 High >/= 190 Very High |
| Classification of Total Cholesterol levels | < 200 Desirable 200-239 Borderline High >/= 240 High |
| Classification of HDL levels | <40 Low >/=60 High (negative risk factor) |
| Lipid Screening Recommendations | Every 5 years beginning at age 20 for those who smoke, have diabetes, or have a hx of heart disease Every 5 years starting at 35 for males and 45 for females |
| Nonpharmacologic Management of Hyperlipidemia | Therapeutic lifestyle changes: Nutrition, Weight reduction, Increased physical activity Patient education regarding risk factors, lifestyle modifications, diet, exercise, etc |
| Pharmacological Management of Hyperlipidemia | Statins Bile Acid Sequestrants Nicotinic Acid Fibric Acids Cholesterol Absorption Inhibitor |
| Statins in Hyperlipidemia | Inhibit HMG-CoA, the enzyme which is partly responsible for cholesterol synthesis Liver func test before starting, then at 6 and 12 wks, and after dose increase In conjuction with diet, exercise, & weight reduction in over weight pts |
| Bile Acid Sequestrants in Hyperlipidemia | Bind bile acids in the intestine which prevents their absorption. These insoluble bile acid complexes are excreted in feces Used to lower LDL in conjunc with diet May prevent absorption of fat soluble vitamins (A, D, E, & K) and many oral meds. Monitor for constipation and flatulence |
| Fibric Acids in Hyperlipidemia | Increase lipolysis and elimination of triglyceride rich particles from plasma, resulting in lower LDL. Gemfibrozil (a FA) given with statins can produce rhabdomyolysis and acute renal failure. Increase risk of gallstone formation Monitor liver func studies and glucose during therapy; both may be elevated |
| Niacin in Hyperlipidemia | Thought to decrease hepatic VLDL production; VLDL is converted to LDL Monitor liver function studies before starting treatment, at 6 & 12 wks, with each dose increase, and periodically Monitor for myalgias and rhabdomyolysis Causes flushing and hypotension |
| Cholesterol Absorption Inhibitor | Inhibit absorption of cholesterol by the small intestine. Can be used alone or with a Statin GI complaints are most common Not necessary to monitor liver function unless concurrently with another med requiring LFT monitoring |
| Pregnancy/Lactation Considerations with Hyperlipidemia | Cholesterol levels are usually elevated during pregnancy Treatment is contraindicated |
| Considerations for Special Populations with Hyperlipidemia | Elderly: Benefits seen with total cholesterol and LDL reduction Statins typically well tolerated by elderly Diabetics: Aggressive management of hyperlipidemia needed |
| Follow up for Hyperlipidemia | Evaluate lipid levels every 5 years starting at age 20 if normal values obtained |